Posts Tagged ‘rare diseases’
What is a Rare Disease?
- By Dr. Priyom Bose, Ph.D.Reviewed by Emily Henderson, B.Sc.
Any unusual life-altering complication of the human body affecting a small number of people is classified as a rare disease (RD). These diseases are complex and possess a significant challenge both in terms of diagnosis and management. The field of rare diseases is constantly evolving.
A plethora of rare conditions are constantly being added to the already existing pool of rare complications. Due to this, clinicians and researchers across the globe are working tirelessly to create better management and therapeutic approaches for the patients.
Image Credit: valiantsin suprunovich/Shutterstock.com
Rare Disease (Looking Deeper)
Compared to the innumerable number of patients affected by prevalent diseases like diabetes, heart diseases, etc., a rare disease has a limited number of patients. So far, about 5000-8000 unique, rare diseases have been described. Rare diseases affect approximately 400 to 700 million individuals globally, making them a global healthcare issue.
An RD affects around 60 million individuals in the United States and the European Union. The number of RDs is currently estimated to be in the thousands. These conditions are frequently significant, harm one’s quality of life, and can even be fatal. Most RDs have a genetic component, with 72–80 % of these disorders having a gene or genes identified.
They are usually defined by their low frequency, measured in terms of prevalence or incidence within a country or geographical region. In the medical literature, five novels RDs are characterized on average every week. According to a global study of RD terminology, 58% of definitions contained a prevalence criterion, with a global average of 40 cases per 100,000 persons.
According to the European Medicines Agency or EMA, rare diseases can be described as a medical condition with a prevalence of fewer than 5 patients in 10,000 people. The research and clinical development surrounding rare diseases are escalating at a positive rate. However, there is a lot more to explore and understand.
The Various Challenges
RDs encompass a wide range of disorders and clinical manifestations, however, the vast majority of RDs afflict children and are chronic and life-threatening. The majority of rare diseases aren’t curable, with only a few having efficient available therapies. The recognition and diagnosis of RDs present several interrelated issues. They significantly impact the quality of epidemiologic and clinical investigations and complicate the definition of unmet patient requirements, safety, possible efficacy, effectiveness, and value of RD treatments.
Inadequate awareness and knowledge of RDs can lead to misdiagnosis and a delay in receiving a definitive diagnosis. Patients who are unfamiliar with relevant signs and symptoms may fail to seek medical help when necessary. Similarly, professionals may misdiagnose the disease or mistake symptoms for those of more frequent diseases with which they are more familiar. The comparability of data from epidemiologic and clinical investigations may be significantly limited if we don’t fully grasp the disease and its cause.
Heterogeneity in pathogenesis, presentation of signs and symptoms, disease severity, and development might make it difficult to characterize a rare disease in clinical research and detect it in ordinary clinical practice, leading to misdiagnosis and underestimating of genuine disease frequency.
In patients with pathognomic clinical characteristics, diagnosing an RD may be simple. Diagnostic certainty, on the other hand, might be a challenge due to the variety of many RDs and the difficulty in correctly interpreting sophisticated investigative testing methods.
Biotechnology eBook Compilation of the top interviews, articles, and news in the last year.
Misdiagnoses are widespread as a result of the aforementioned issues, which can lead to ineffective therapy. Such medication may not only cause adverse effects, but it may also hide signs of the underlying problem, delaying the accurate diagnosis and beginning of suitable treatment even longer. An RD’s occurrence varies by geography and country, ranging from dense clustering in certain areas to vast distribution in others. In the situation of prevalence heterogeneity, prevalence statistics from epidemiologic studies undertaken in a specific region may be incorrectly extrapolated to larger geography.
Overcoming the hurdles
Rare disease research has received a great deal of attention in recent decades. It is primarily due to legislation designed to make it easier for patients to have access to effective treatments by rewarding pharmaceutical and biotechnology companies to develop novel medications that would otherwise be unprofitable. In the field of rare diseases, there has also been a remarkable increase in social awareness and worldwide connectedness. Several groups are forming to provide information to the general public and to educate them about uncommon diseases.
As a result, governments all over the world have realized the importance of enacting laws and regulations to encourage the development of new and novel technology for the treatment of RDs. The detection of RDs has improved due to advancements in molecular genetics, disease pathophysiology, and medical technology. They’ve also aided researchers in figuring out how to improve the diagnosis, prognosis, treatment for rare diseases and precisely subclassify common diseases into groups of RDs with different characteristics.
Patient Registries for Rare Diseases: A Goldmine
Patient registries are a valuable instrument in the field of rare diseases (RD) that aids clinical research, promotes the development of appropriate clinical trials, improves patient care, and supports healthcare administration. They create a critical information infrastructure that supports the work of European Reference Networks (ERNs) on rare diseases.
There has been a significant expansion of RD registries in recent years, necessitating the development of guidance for the basic requirements, recommendations, and standards required to maintain a high-quality registry. Several such registries have been formed in recent years including, the Registry for Neuromuscular Disease, Central Registry of Rare Diseases (CRRD), Ataxia-Telangiectasia International Registry, EHDN: registry of juvenile Huntington’s disease, and EUROCARE CF: European cystic fibrosis registry.
The Rare Diseases Registry Program (RaDaR) website was developed in 2021 by NCATS to give the rare disease community free and easily available instructions on how to set up and manage high-quality registries. RaDaR will be a dynamic website. In a staged approach, NCATS staff will continue to add new instructions, best practices, testimonials, and other resources from the rare disease community to the site. Although the researchers exploring the area of rare diseases have achieved significantly, we still have a long road ahead of us.
References:
- Navarrete-Opazo, A. A., Singh, M., Tisdale, A., Cutillo, C. M., & Garrison, S. R. (2021). Can you hear us now? The impact of health-care utilization by rare disease patients in the United States. Genetics in medicine: official journal of the American College of Medical Genetics, 23(11), 2194–2201. https://doi.org/10.1038/s41436-021-01241-7
- Nestler-Parr, S., Korchagina, D., Toumi, M., Pashos, C. L., Blanchette, C., Molsen, E., Morel, T., Simoens, S., Kaló, Z., Gatermann, R., & Redekop, W. (2018). Challenges in Research and Health Technology Assessment of Rare Disease Technologies: Report of the ISPOR Rare Disease Special Interest Group. Value in health: the journal of the International Society for Pharmacoeconomics and Outcomes Research, 21(5), 493–500. https://doi.org/10.1016/j.jval.2018.03.004
- Kodra, Y., Weinbach, J., Posada-de-la-Paz, M., Coi, A., Lemonnier, S. L., van Enckevort, D., Roos, M., Jacobsen, A., Cornet, R., Ahmed, S. F., Bros-Facer, V., Popa, V., Van Meel, M., Renault, D., von Gizycki, R., Santoro, M., Landais, P., Torreri, P., Carta, C., Mascalzoni, D., … Taruscio, D. (2018). Recommendations for Improving the Quality of Rare Disease Registries. International journal of environmental research and public health, 15(8), 1644. https://doi.org/10.3390/ijerph15081644
- Richter, T., Nestler-Parr, S., Babela, R., Khan, Z. M., Tesoro, T., Molsen, E., Hughes, D. A., & International Society for Pharmacoeconomics and Outcomes Research Rare Disease Special Interest Group (2015). Rare Disease Terminology and Definitions-A Systematic Global Review: Report of the ISPOR Rare Disease Special Interest Group. Value in healt : the journal of the International Society for Pharmacoeconomics and Outcomes Research, 18(6), 906–914. https://doi.org/10.1016/j.jval.2015.05.008
- Griggs, R. C., Batshaw, M., Dunkle, M., Gopal-Srivastava, R., Kaye, E., Krischer, J., Nguyen, T., Paulus, K., Merkel, P. A., & Rare Diseases Clinical Research Network (2009). Clinical research for rare disease: opportunities, challenges, and solutions. Molecular genetics and metabolism, 96(1), 20–26. https://doi.org/10.1016/j.ymgme.2008.10.003
- RaDaR. [Online] National Center for Advancing Translational Sciences. Available at: https://ncats.nih.gov/radar
Last Updated: Feb 15, 2022
Europe Approves Avapritinib for Rare Mast Cell Disease
Drishti Agarwal
December 13, 2023
The European Commission has granted approval to avapritinib (Ayvakyt) to address moderate to severe symptoms in adult patients with indolent systemic mastocytosis (ISM) who are inadequately managed by current symptomatic treatments. This marks the first approved therapy for individuals with the condition in Europe.
ISM is a rare blood disorder characterized by an abnormal build-up of neoplastic mast cells in the bone marrow and other organs, including the skin. It is accompanied by often distressing symptoms like pruritus, flushing, syncope, headache, vomiting, diarrhea, and abdominal pain. It affects around 40,000 individuals in the European Union.
Avapritinib is a kinase inhibitor that was developed to selectively target the disease’s key driver, the KIT D816V mutation in mast cells.
After the favorable recommendation from the Committee for Medicinal Products for Human Use in November 2023, the European Commission’s decision to approve avapritinib is grounded in data from the PIONEER trial.
The phase 2 trial found significant and clinically relevant benefits from the use of avapritinib plus best supportive care (BSC) medicines in patients with symptomatic ISM. This was true across various efficacy assessments, encompassing both disease symptoms and the burden of pathologic mast cells.
The first part of the trial established the recommended dose of 25 mg once daily. The second part compared avapritinib 25 mg once daily plus BSC against placebo plus BSC in patients with moderate to severe ISM. The third part is an ongoing open-label extension that is evaluating avapritinib 25 mg once daily for up to 5 years.
So far, avapritinib has been found to lead to significant improvements compared with placebo across primary and all pivotal secondary measures, which were evaluated from baseline to 24 weeks (part 2) and has demonstrated intensified efficacy through 48 weeks of treatment (part 3). Overall, 96% of patients receiving avapritinib completed 24 weeks of treatment and opted to cross over to part 3. The detailed results were published in NEJM Evidence.
In part 2, 212 patients with moderate to severe ISM were randomly assigned to receive oral avapritinib 25 mg once daily (n = 141) or placebo (n = 71) across 42 sites in 13 countries. Compared with the placebo group, the avapritinib group had a significantly greater decrease in the total symptom score (TSS; 15.6 vs 9.2 points; P < .003) and showed a significantly higher rate of achieving a 50% or greater reduction in serum tryptase levels (P < .001).
In part 3, for the crossover patients who finished an extra 24 weeks of treatment (n = 26), the average shift in TSS at 48 weeks was -21.4. Approximately 37% experienced reductions of 50% or greater in TSS, and approximately 59% showed a 30% or greater reductions within around 4 months.
Avapritinib was also well-tolerated, presenting a favorable safety profile, with the severity of most reported adverse events categorized as mild. Common adverse events included flushing, edema, increased blood alkaline phosphate, and insomnia.
In Europe, plans are underway for the initial commercial launch in Germany, followed by subsequent market introductions determined by the respective local healthcare technology assessment and reimbursement timelines.
https://www.medscape.com/viewarticle/europe-approves-avapritinib-rare-mast-cell-disease-2023a1000vb3
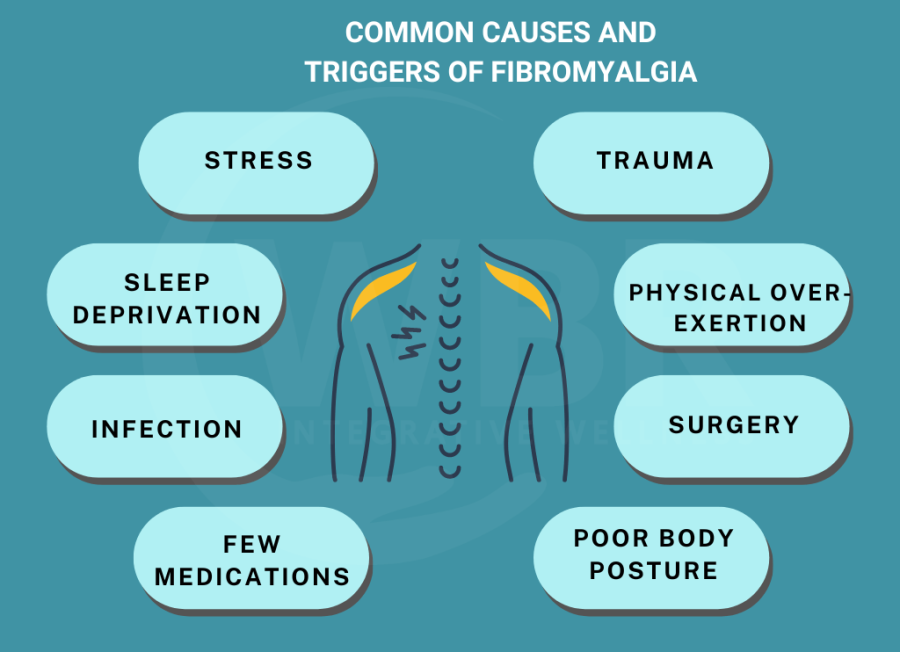
Traditional CBT as effective as exposure therapy for fibromyalgia
There does not appear to be any profound differences between so-called exposure-based CBT and traditional CBT in the treatment of fibromyalgia, according to a study led by researchers at Karolinska Institutet. Both forms of treatment produced a significant reduction in symptoms in people affected by the disease. The study is one of the largest to date to compare different treatment options for fibromyalgia and is published in the journal PAIN.
About 200,000 people in Sweden currently live with fibromyalgia, a long-term pain syndrome that causes great suffering for patients through widespread pain, fatigue, and stiffness in the body. There is no cure for fibromyalgia. Existing drugs often have insufficient effect, raising the need for more effective treatment methods. Cognitive behavioral therapy (CBT) has shown some effect, but there is a lack of trained CBT practitioners. There is also a lack of knowledge about which form of CBT is most effective.
The study compared two different forms of internet-delivered cognitive behavioral therapy in terms of how well they reduce the symptoms and functional impact of fibromyalgia.
In brief, exposure-based CBT involves the participant systematically and repeatedly approaching situations, activities, and stimuli that the patient has previously avoided because the experiences are associated with pain, psychological discomfort, or symptoms such as fatigue and cognitive problems.
In traditional CBT, the participant is presented with several different strategies to work on during treatment, such as relaxation, activity planning, physical exercise, or strategies for managing negative thoughts and improving sleep.
The study showed that traditional CBT was by and large equivalent to the newer treatment form of exposure-based CBT.
The randomized study involved 274 people with fibromyalgia, who were randomly assigned to be treated with traditional or exposure-based CBT. The treatments were delivered entirely online and all participants had regular contact with their therapist.
Participants answered questions about their mood and symptoms before, during, and after treatment. After the 10-week treatment, 60 percent of those who received exposure-based CBT and 59 percent of those who received traditional CBT reported that their treatment had helped them.
“The fact that both treatments were associated with a significant reduction in the participants’ symptoms and functional impairment and that the effects were sustained for 12 months after completion of the treatment, indicates that the internet as a treatment format can be of great clinical benefit for people with fibromyalgia,” says Maria Hedman-Lagerlöf. “This is good news because it enables more people to access treatment.”
The study is the second largest to compare different psychological treatment options for fibromyalgia, according to the researchers.
“Our study is also one of the first to compare with another active, established psychological treatment,” says Maria Hedman-Lagerlöf.
The study was a collaboration between Karolinska Institutet and Uppsala University. It was financed by The Bank of Sweden Tercentenary Foundation and none of the researchers have declared any conflicts of interest.
UB research identifies key mechanism in infantile cystinosis
University at Buffalo research has identified how a misstep in the genesis of a key component of the kidney causes infantile cystinosis, a rare disease that significantly shortens the lifespan of patients. Published Nov. 30 in the International Journal of Molecular Sciences, the work reveals that the mechanisms that cause the disease could be addressed and potentially cured through the genome-editing technique CRISPR. That could make kidney transplants, the most effective treatment currently available for these patients, unnecessary.
Infantile cystinosis, the most common and most severe type of cystinosis, occurs as the result of an accumulation in the body’s cells of cystine, an amino acid. The buildup damages cells throughout the body, especially the kidneys and the eyes. Treatment consists of medications that work to lower the level of cystine in the body, as well as therapies that address the impaired growth of these children due to the inability to properly absorb nutrients. Some children require feeding tubes. Eventually, patients with infantile cystinosis, also called nephropathic cystinosis, will require dialysis and a kidney transplant.
Promise of stem cells
Human-induced pluripotent stem cells (hiPSCs) are stem cells that can differentiate into many different cell types. They hold tremendous potential for studying genetic diseases; the drawback has been that differentiation into certain cell types has been problematic. Such is the case with many cell types found in the kidney.
But a new protocol developed by this research team was successful.
Ramkumar Thiyagarajan, PhD, assistant professor of geriatric studies at the University of Kansas and formerly a postdoctoral fellow at UB, is first author on the paper.
The protocol involved extracting stem cells from a healthy individual and an individual with infantile cystinosis. The researchers developed a culture medium to grow stem cells that included a small number of defined components present in blood, including insulin, specific proteins, growth factors and others. “Conducting the differentiation protocol under these conditions occurred in a timely manner,” says Taub, “we didn’t have to wait for weeks on end, and it occurred in a reproducible manner.”
The researchers were able to efficiently differentiate the hiPSCs into the kidney proximal tubule, the type of nephron in the kidney that is impaired in infantile cystinosis, as well as in other kidney diseases.
“Unlike in other studies, we were able to retain a number of markers in the tubule that are physiologically important in the kidney’s reabsorptive functions,” says Taub. “Although these markers were expressed in both the normal and the cystinosis-derived hiPSCs, the genesis of the tubule was impaired in the cystinosis-derived cells, mimicking what happens in infantile cystinosis.”
A potential cure
That finding means that the CRISPR genome-editing technique could be used to repair the defective genome and potentially cure the disease. “The normal gene can be introduced in the genome of cystinotic hiPSCs, which can then be injected in the kidney to replace the defective proximal tubules of individuals with infantile cystinosis,” Taub says.
“In cystinotic individuals, it is the renal proximal tubule that degenerates, presumably due to programmed cell death,” explains Taub, “so the entire kidney would not need to be replaced. The defective renal proximal tubules of individuals with this disease can be replaced with normal tubules following the introduction of the normal gene into cystinotic hiPSCs obtained from the patient. And because these tubules are from cells derived from the patient, there should be no problem with tissue rejection.”
The findings are applicable to other kidney diseases where the renal proximal tubule is damaged, including acute kidney injury that can lead to chronic kidney disease and renal failure, and can be fatal.
Initial studies will need to be conducted with animal models as well as with in vitro tissue culture cells.
The research was funded by UB’s WNYSTEM and The Cystinosis Research Foundation.
Source:
Journal reference:
Thiyagarajan, R & Taub, M. (2023). Studies with Human-Induced Pluripotent Stem Cells Reveal That CTNS Mutations Can Alter Renal Proximal Tubule Differentiation. International Journal of Molecular Sciences.